Gain knowledge & leverage to increase Medicare Advantage reimbursement
A must-have to find good payers & negotiate your MA contracts:
Monitor the utilization of Medicare Advantage in every local market:
Calibrate payer reported rates with your contracts and recent claims:
Instantly synchronize payer rates and
terms to your current systems
Select a State and/or County to identify the which payers have the most seniors enrolled in Medicare Advantage (hover for more details)
Our team has deployed software in thousands of nursing homes. We know you are tired of having to remember dozens of passwords.
Payer Clariti brings payer insights and knowledge to you, where you work. We'll set up your markets, the competitors you want to watch and keep you aware of the changes happening in Medicare Advantage.
Create a Payer Clariti account and add your users.
You can set up alerts to monitor payer rates in your locations & share market updates with your team.
Based on your added facility locations, Payer Clariti discloses known payer rates for all facilities in their market.
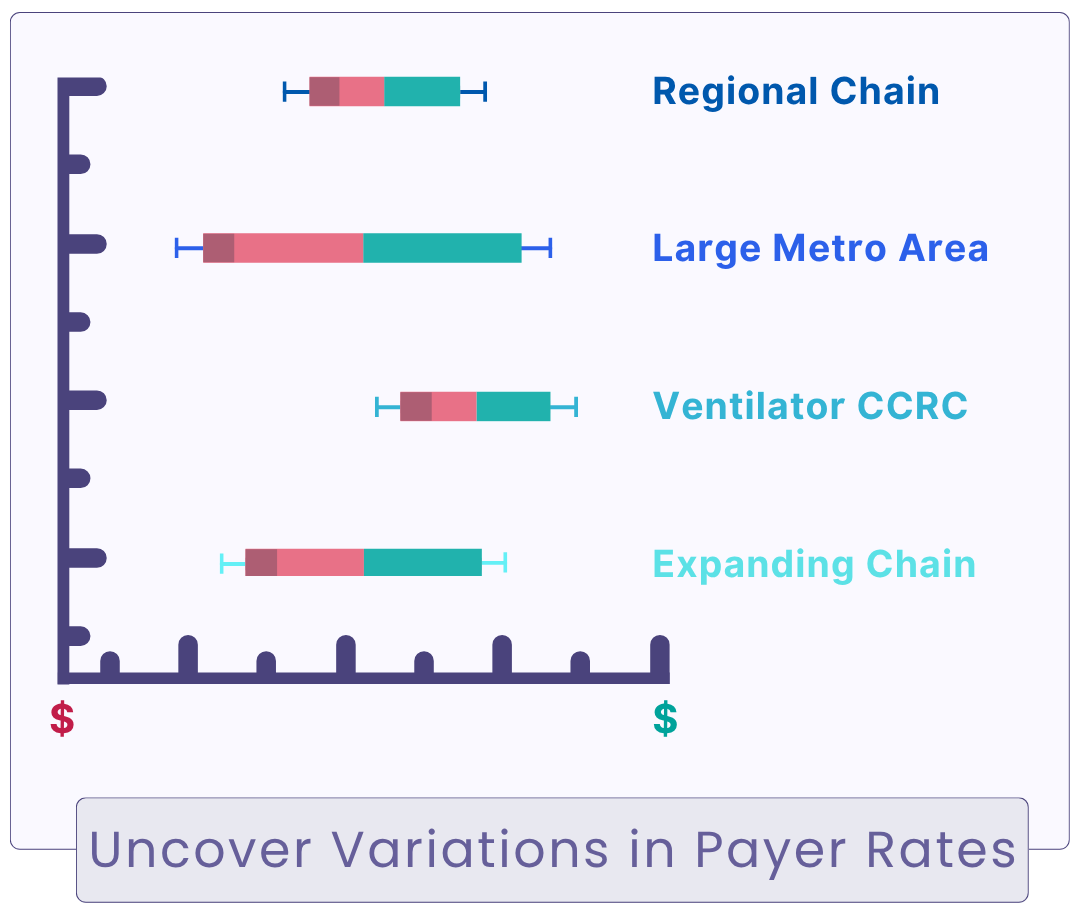
We've built reports to help you explore rates by locations, chain operators, Five Star ratings and much more. You can find the data you want - and set up regular notifications of rate changes.
With recent scrutiny, Medicare Advantage payers are exiting markets and changing strategies.
Payer Clariti monitors payer filings to show you where enrollments and payer share is changing so you can plan accordingly.
Import your payer agreement PDF's or recent claims and Payer Clariti reconciles them to payer published rates - showing you anything inconsistent.
Start for free and see if Payer Clarity can help!